Study finds evidence of COVID-19 in air, on hospital surfaces
Filed Under: COVID-19
Stephanie Soucheray | News Reporter | CIDRAP News
| Apr 13, 2020
A study published late last week in Emerging Infectious Diseases found a wide distribution of COVID-19 virus genetic material on surfaces and in the air about 4 meters (13 feet) from patients in two hospital wards in Wuhan, China, posing a risk to healthcare workers.
While the findings of the environmental sampling study do not indicate the amount of live virus, if any, or precisely determine the distance of aerosol transmission, the authors say that they confirm that the virus spreads in aerosols in addition to large respiratory droplets.
The researchers tested surface and air samples from an intensive care unit (ICU) and general coronavirus ward at Huoshenshan Hospital from Feb 19 to Mar 2 to detect evidence of SARS-CoV-2, the coronavirus that causes COVID-19.
Fifteen patients were in the ICU, while 24 were housed in the general ward. The investigators used quantitative real-time polymerase chain reaction to identify virus in swabs of floors, computer mice, trash bins, bed handrails, patients’ face masks, health workers’ personal protective equipment, and air vents.
Nearly all (54 of 57) positive samples (94.7%) were from contaminated areas of the ICU and general ward (9/9 [100%]). Rate of positive samples was much higher for the ICU than for the general ward (54/124 [43.5%] vs. 9/114 [7.9%]).
Virus aerosols in ICU
Fourteen of 40 air samples from the ICU (35%) tested positive for coronavirus, while 2 of 16 from the general ward (12.5%) were positive. Eight of 12 ICU air vent swabs (66.7%) tested positive, as did 1 of 12 (8.3%) general ward swabs, results that the authors said “confirm that SARS-CoV-2 aerosol exposure poses risks.”
COVID-19 aerosol was found near air vents (5/14 [25.7%]), in patient rooms (8/18 [44.4%]), and in the doctor’s office area (1/8 [12.5%]), indicating that aerosolized virus was concentrated near and downstream of patients. However, the upstream area also posed a risk and that, based on the detection of virus in the doctor’s office, “the maximum transmission distance of SARS-CoV-2 aerosol might be 4 m,” they said.
Using the aerosol test results, the researchers identified the patient care area of the ICU as high risk because of the high positivity rate (13/32 [40.6%]). “Thus, stricter protective measures should be taken by medical staff working in the ICU,” the authors said.
Contaminated shoes, computer mice, bedrails
The relatively high rate of positivity for floor samples in the ICU (7/10 [70%] and general ward (2/13 [15.4%] may have been due to gravity and air flow causing most respiratory droplets to fall to the ground and spread via clinicians’ shoes, the authors surmised, noting a 100% positivity rate on the pharmacy floor, where no patients were housed and three samples were taken.
Half of the swabs from the soles of clinicians’ shoes tested positive, indicating that the virus may spread this way. “We highly recommend that persons disinfect shoe soles before walking out of wards containing COVID-19 patients,” they said.
The highest rates of positivity from objects came from computer mice (6/8 [75%] in the ICU; 1/5 [20%] in the general ward), trash cans (3/5 [60%] in the ICU; 0/8 in the general ward), bed handrails (6/14 [42.9%] in the ICU; 0/12 in the general ward); and doorknobs (1/12 [8.3%] in the general ward).
Patient masks had a high rate of positivity because they contained exhaled droplets and saliva, which the authors said suggests that the masks should be disinfected before disposing of them. Some positive results came from clinicians’ sleeve cuffs and gloves, which the researchers said indicates that staff should wash their hands immediately after patient contact.
As of Mar 30, no hospital employees had tested positive for COVID-19, which may be partially attributed to China’s use of mobile hospitals in Wuhan, “which ensured that all patients with suspected disease were cared for by professional medical staff and that virus transmission was effectively cut off,” they wrote.
https://www.cidrap.umn.edu/news-perspective/2020/04/study-finds-evidence-covid-19-air-hospital-surfaces
Stephanie Soucheray | News Reporter | CIDRAP News | Apr 13, 2020 A study published late last week in Emerging Infectious Diseases found a wide distribution of COVID-19 virus genetic material on surfaces and in the air about 4 meters (13 feet) from patients in two hospital wards in Wuhan, China, posing a risk to healthcare workers. While the findings of the environmental sampling study do not indicate the amount of live virus, if any, or precisely determine the distance of aerosol transmission, the authors say that they confirm that the virus spreads in aerosols in addition to large respiratory droplets. Sounds like an argument for avoiding being quarantined with infected persons, Why hospitals are hotbeds of coronavirus transmission , versus a practice shown to be efficacious during the 1918 flu:
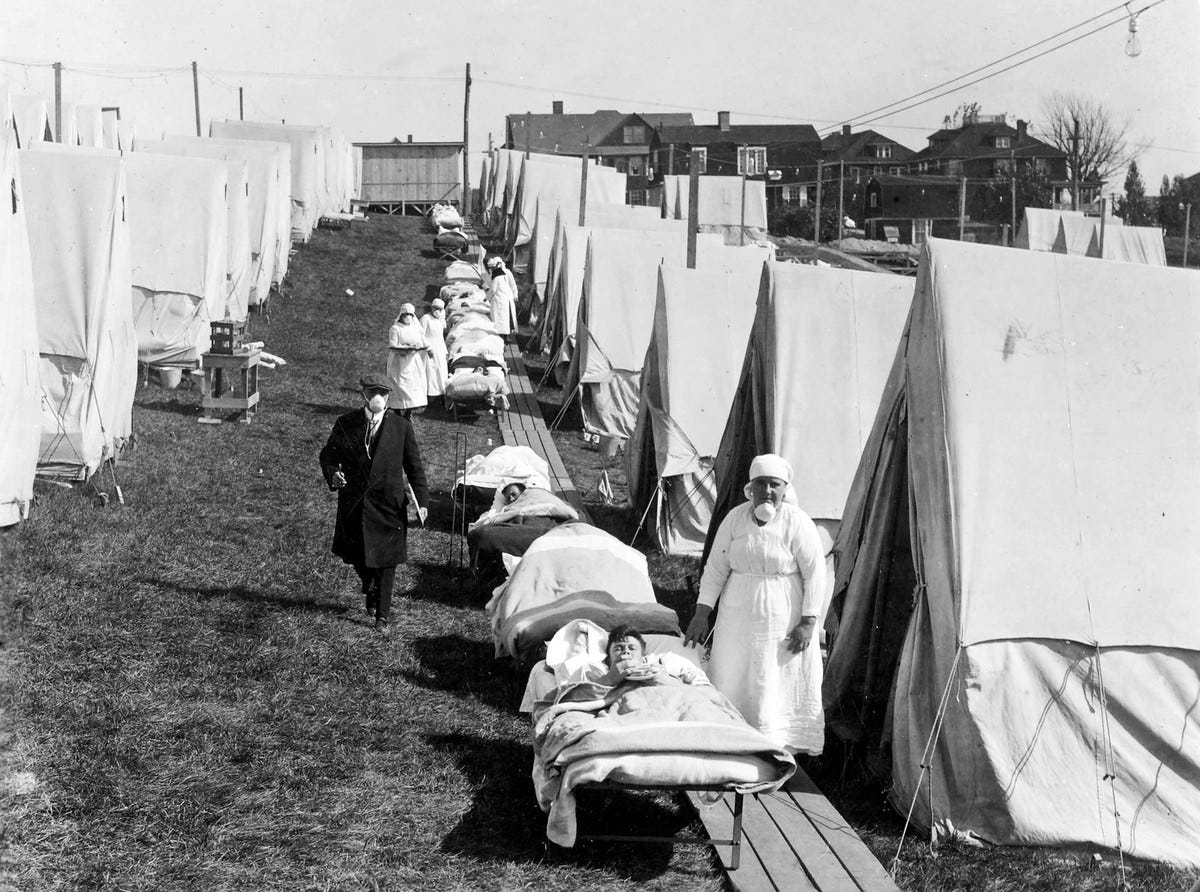
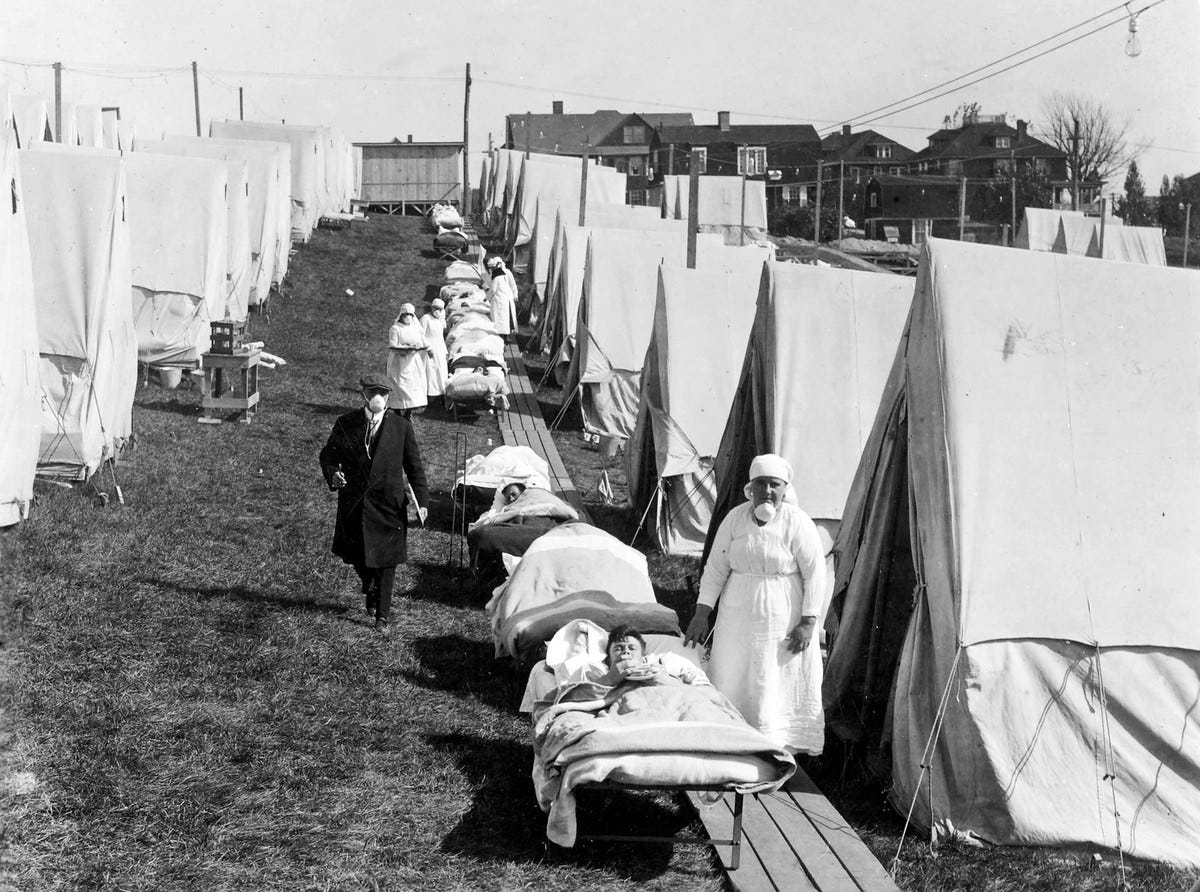
https://medium.com/@ra.hobday/coronavirus-and-the-sun-a-lesson-from-the-1918-influenza-pandemic-509151dc8065 Coronavirus and the Sun: a Lesson from the 1918 Influenza Pandemic . Put simply, medics found that severely ill flu patients nursed outdoors recovered better than those treated indoors. A combination of fresh air and sunlight seems to have prevented deaths among patients; and infections among medical staff.
`Open-Air’ Treatment in 1918 During the great pandemic, two of the worst places to be were military barracks and troop-ships. Overcrowding and bad ventilation put soldiers and sailors at high risk of catching influenza and the other infections that often followed it.[2,3] As with the current Covid-19 outbreak, most of the victims of so-called `Spanish flu’ did not die from influenza: they died of pneumonia and other complications.
However, A Virologist Explains Why COVID-19 Coronavirus Isn’t Really Dangerously Lingering On Surfaces For Weeks
But, COVID-19 may spread through breathing and talking — but we don't know how much